
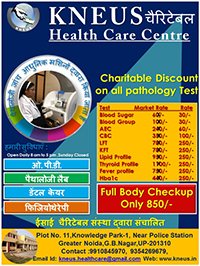
KNEUS an NGO run by the Christian Charitable Organization With its main purpose, it has been contributing to the various health services of the society for about thirty years. Now KNEUS has taken a significant step in the field of health awareness and health care activities especially for the poor and needy. KNEUS through various approach and efforts for better health care services provides in the society. KNEUS has installed a complete Automatic Pathology Lab in the Head office Greater Noida. KNEUS also has sample collection centres have been kept in Sec-10,Noida and Salarpur. So that more and more needy people can get better services. This Pathology Lab provides unique quality and services to our customers. In the Lab different types of tests and molecular diagnosis, serology, immunocomistry, PCR technology, infectious diseases, biochemistry, hematology etc..Under the supervision of experience personnel and pathologist. KNEUS has been organizing Free Health Check-up Camps in order to raise mass awareness about health and the importance of regular health check-ups. A collection center is place where a customer walks-in and gives his sample with belief and confidence on KNEUS’s accuracy and efficiency. KNEUS will continue to move the fulfilling of their services on the basis of their mission.
Our aim:
1- Providing good quality diagnostic pathology investigations.
2- Providing pathology check-ups at cheap rates to the needy and poor people.
3- Participation in the creation of a healthy and happy society
LEAVE NO ONE BEHIND-United to End TB
Tuberculosis (TB) is a major public health problem in India. India accounts for one-fifth of the global TB incident cases. Each year nearly 2 million people in India develop TB, of which around 0.87 million are infectious cases. It is estimated that annually around 330,000 Indians die due to TB. One Tuberculosis patient spreads it to 15 people.
Since 1993, the Government of India (GoI) has been implementing the WHO-recommended DOTS strategy via the Revised National Tuberculosis Control Programme (RNTCP). The WHO-recommended Directly Observed Treatment, Short Course (DOTS) strategy was launched formally as Revised National TB Control programme in India in 1997 after pilot testing from 1993-1996. We have partnered with RNTCP for implementing the RNTCP TB programme at State and District level in India. RNTCP recognizes the need for involvement of all sectors –public and private
To create an epidemiological impact of Tuberculosis control .The private health sector in the country is an important source of care even with the availability of public health services. The NGOs and private providers are often closer to and more trusted by patients and perform an active role in health promotion in the community.
Public private mix (PPM) has been recognized as an important component in the RNTCP. The aim of public private mix-DOTS (PPM-DOTS) is to effectively link the national TB programme and all public and private health care providers presently out of realms of national TB programme efforts so as to provide standardized treatment to all TB patients in the country. The Government of India developed guidelines for NGO and private sector involvement in TB control which were published in 2000 and 2001 respectively. Today, PPM in RNTCP has come a long way with a support of over 2500 NGOs, 25000 PPs, 260 Medical colleges and 150 corporate houses which are providing DOT services.We have Partnership under Option 2.b. Designated Microscopy cum Treatment Centre in Revised National Tuberculosis Control Programme.
Our approach focuses on the diagnosing, registration of the patient and medical supply (DOTS) in the urban, rural, poorest and most remote locations. We work directly with government agencies, adhering to the guidelines issued by WHO and the Government of India, to ensure sustainability of the treatment.
FACT ABOUT TB :
TB is an abbreviation of the word Tuberculosis and is how people often refer to the disease. TB is a disease caused by bacteria called Mycobacterium tuberculosis.
LATENT TB:
The bacteria that usually cause the disease in humans, usually affect the lungs, but can affect other parts of the body. If you are infected with the bacteria you won’t necessarily become sick, because you can have either latent TB or TB disease. People with latent TB do not feel sick and do not have any symptoms.
Under nutrition increases the likelihood of latent TB infection progressing to active TB disease.
TB DISEASE:
TB disease is what happens when a person has latent TB and then becomes sick. Sometimes this is known as having active TB. Overall about 5 to 10% of people with latent TB, who do not receive treatment for it, will become sick at some time in their lives.
Some people become sick soon after they have become infected, before their immune system (the part of the body that fights diseases) can fight the bacteria. Other people don’t get sick at first but they get sick years later when their immune system becomes weak for another reason. This can be because they have an infection, such as HIV, or some other health problem.
Some people are known to have a higher risk of becoming ill.
These include :
- Infants and children aged less than 4 years
- People infected within the previous two years
- People infected with HIV
- People who have certain illnesses or conditions which affect their immune system, such as people with diabetes, and people with chronic renal failure.
WHAT ARE THE SYMPTOMS OF TB?
The symptoms depend on which area of the body has been infected. If someone has pulmonary disease, which is TB in the lungs, then they may have a bad cough that lasts longer than two weeks. They may also have pain in their chest and they may cough up blood or phlegm from deep inside their lungs. Other symptoms of TB include weakness or fatigue, weight loss, lack of appetite, chills, fever and night sweats.
DIAGNOSING TB:
It is very difficult to diagnose TB by a person’s symptoms on their own. This is because some other diseases have the same symptoms.
A diagnosis is usually only certain when there is definite evidence of TB bacteria. Some of the TB tests used for diagnosis look directly for the bacteria. Others such as the chest X-ray look for the effect of the bacteria on the person suspected of having TB. Tests for diagnosis include the TB skin test, sputum microscopy, the culture test as well as the new Gene-xpert test.
Major problems with the older tests are the lack of accuracy as well as the time they take. With newer tests a major issue is the cost.
TREATMENT:
TB can usually be cured and more than twenty drugs have been developed for treating TB. But most of the drugs were developed many years ago. The treatment usually consists of a combination of TB drugs that must be taken for at least six months. But the treatment will only be successful if the drugs are taken exactly as required for the entire length of time.
The drugs are used in different combinations in different circumstances. For example, the five “first line” drugs are given to people who have never had treatment before. If people have had treatment before they may need to take second line drugs.
Some of the drugs have very severe side effects and are very difficult to take for such a long period of time. This is why there is an urgent need for new TB drugs to be developed. In addition many people are now resistant to one or more of the drugs.
There is a two way link between TB & nutrition. TB makes under nutrition worse, and under nutrition makes TB worse.
DRUG RESISTANT TB
If someone has drug resistant TB it means that the bacteria in their body won’t be affected by certain drugs that they are resistant to. The drugs just won’t work. There are two main reasons why people develop it. It can be because the person doesn’t take their drugs properly. It can also be that the bacteria that they are infected with, have come from someone who has already got drug resistant TB. Being drug sensitive is the opposite of being drug resistant.
If someone has drug resistant TB then they must change drugs. But usually they mustn’t have just one new drug. They need to have several new drugs and for it to be believed that they will all be effective. Drug susceptibility testing which is available in many countries, and is very important, provides information about which drugs a person is resistant to.
PREVENTION:
A major part of the prevention of TB is to stop the spread of bacteria from one adult to another. This is done by firstly finding the adults who have TB. Then providing them with effective treatment which means that they are no longer infectious, and they will also usually then recover from being sick. There is a vaccine, the BCG vaccine, but it is used for children as it doesn’t seem to prevent the disease in adults. TB infection control is also important to prevent people from getting infected in health care facilities.
Sometimes it is believed that education only needs to involve people who already have the disease. But there is also a need to educate the general public. This is to ensure that people know how the disease is spread, and also to reduce the stigma surrounding the disease. It can also help to ensure that people come forward for testing and treatment as soon as possible.
STATISTICS:
The statistics for TB show how there are very different levels of TB in different parts of the world. Not only national governments, but organizations such as the World Health Organization (WHO) are making significant efforts to End TB.
The countries known as the high burden countries are those with the highest level of disease. They include India, Indonesia, China and Nigeria. Many countries are now making greater efforts to combat TB. In India the government recently announced that its aim is to eradicate the disease by 2025.
KNEUS was formed for a stupendous task of eliminating leprosy, which was founded by its Ex-Executive Director Rev. Fr. Francis Borgia along with the Regional Bishops of U.P., Rajasthan Region. It was their compelling desire to alleviate the untold sufferings of thousands of leprosy patients living in the Northern States of India that made them form KNEUS to help in the process of eliminating leprosy and bring relief to the population from this dreaded disease that renders a human being a living dead.
KNEUS takes pride in saying that its committed workers till now have detected 49,720 patients, of whom have completed treatment and are cured till March, 2003.
This is besides the thousands who have come from outside the project areas who were treated, thus enabling them to lead a life of dignity and self respect. And our mission will continue until such time that the leprosy patients exist in the country.
KNEUS is still active, doing IEC (Information, Education and Communication) in tune with Government guidelines of SET modified (2004).
According to the WHO report, “The South-East Asia Region, including India, achieved the elimination goal in December 2005.”
But now the fear is finally, in low endemic situations when the disease is no more a public health problem, there is danger of complacency, lessened competency in diagnosing the disease, low priority, low political commitment and inadequate resources.
The observations of late Dr. Sadashiv Tare, an eminent leprosy worker, have been a constant source of inspiration for KNEUS in its spirit of commitment and dedication, who has said, “The first thing to realise would be that leprosy would never be totally eradicated. And the World Health Organisation and Indian Government have made unscientific compromises that have led to under-reporting of cases. It has been undeclared policy of the two agencies to discourage detection and registration of new patients in the race against time. Patients are doled out MDT medicines and asked to consume the course in six months. If they do that, they are supposed to take for granted that they have been cured.”
Our bare exposure to the incidence of leprosy also make us feel and think in the same vein that leprosy will never be eradicated totally and our fight and struggle would continue till we succeed in arresting this dreaded disease.
KNEUS reach out to the people with the campaign like pamphlet distribution, banners, regular tests, separate seminars for the youth, women and men, etc. KNEUS believe in the principle that only 100% awareness of the HIV AIDS can eradicate it rather than treatment. HIV associated tuberculosis remains a major global public health challenge, with an estimated Incidence of HIV-TB in India 87,000 and 1.03 million patients registered worldwide in the year 2017. Co-infection with HIV leads to challenges in both the diagnosis and treatment of tuberculosis. Further, there has been an increase in rates of drug resistant tuberculosis, including multi-drug resistant (MDR-TB) and extensively drug resistant.Which are difficult to treat and contribute to increased mortality. KNEUS have 2 DMC’s in the district GautamBuddh Nagar. All the registered TB patients undergo Integrated Counseling and Testing Centre ICTC for test.